Why safety leaders should know what ototoxicants are and how to eliminate them


You've landed your dream job, you're working hard to make your mark, and suddenly debilitating dizziness and balance issues threaten to take it all away. Tests are inconclusive. The mystery deepens. Is something at work making you sick?
I experienced mysterious balance issues during my first job as a refinery process engineer in the 1980s. It was frustrating and frightening, and led to many months of medical testing (and concern about my health). When the tests were clear, the symptoms were blamed on workload and stress. And while this was plausible, it didn't seem right to me.
I wish that at the time I had known more about a group of common chemicals known as ototoxicants.
Exposure to ototoxic substances can damage the delicate hair cells in your inner ear, which are responsible for converting sound vibrations into electrical signals that your brain can interpret as sound.
Symptoms of ototoxicity can vary depending on the type and amount of exposure, but they may include hearing loss, tinnitus (ringing or buzzing in the ears), dizziness, or problems with balance.
Ototoxicity can result from exposure to a wide range of chemical products in various industries, and the extent of its occurrence can vary significantly depending on factors such as the specific chemicals involved, exposure levels, duration of exposure, and individual susceptibility.
When I started my career, WHMIS was just being introduced. I wore personal protective equipment such as a hard hat, safety glasses and shoes, leather gloves and fire-retardant coveralls, but there wasn’t much knowledge about or protection from the hazards associated with chemical exposures. My leather gloves protected my hands from cuts and injuries, but they provided no protection against chemicals and were often soaked through when handling samples.
Today with more knowledge about ototoxic chemicals and the benefit of hindsight I suspect that my regular exposure to solvents together with high levels of noise were contributing to my symptoms, which resolved once I left refining.
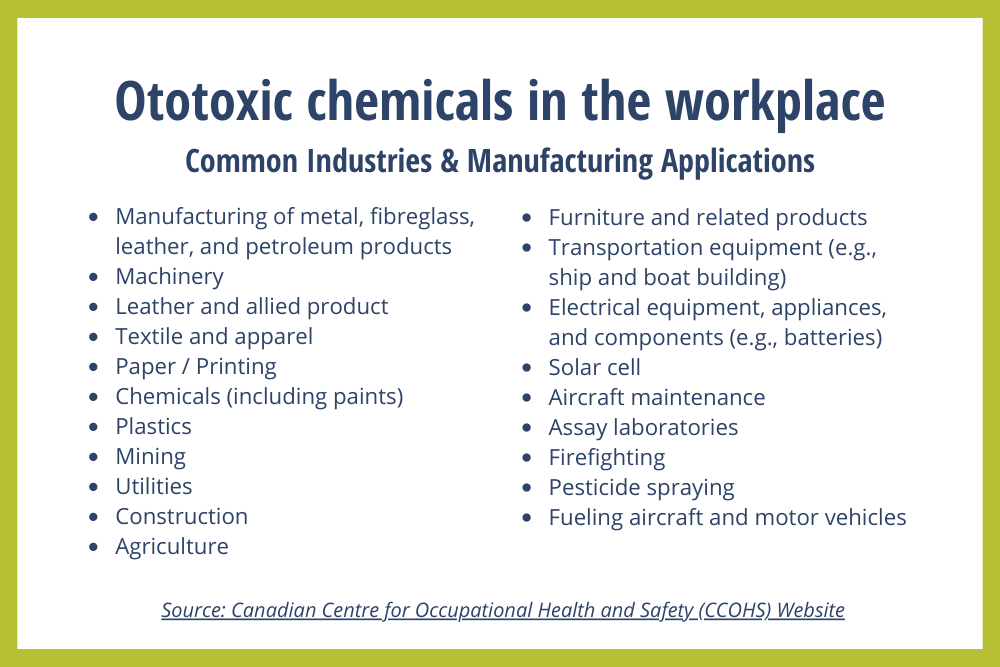
There are more than 100 substances present in workplaces that have been identified as being potentially ototoxic, according to the Canadian Centre for Occupational Health and Safety (CCOHS).
Ototoxic chemicals are found in paints, gasoline, solvents, floor sealers, graffiti remover and many other products used across industries and sectors such as manufacturing, mining, chemical processing, agriculture, utilities, hospitality, municipalities and more.
While it's difficult to gauge how widespread ototoxicity is in the workplace, it is important to note that occupational hearing loss, which includes both noise-induced hearing loss and hearing loss due to chemical exposure, is a prevalent occupational health issue and it often goes unreported or unrecognized.
According to the Centers for Disease Control and Prevention (CDC), occupational hearing loss is one of the most common work-related illnesses in the United States. Statistics Canada data shows that while hearing loss increases with age, as we may expect, the percentage of adults experiencing tinnitus is similar in all age categories.
Ototoxicity prevention
Ototoxicants can be absorbed through the skin or through inhalation; however, the symptoms that result from exposure are difficult to troubleshoot. For example, if an employee experiences hearing loss or tinnitus, the normal course of action for the employer is to conduct sound level readings and ensure hearing protection is provided.
However, with ototoxic chemicals the problem is the quality of air an employee is breathing and whether they are being exposed to high levels of the chemicals. Troubleshooting is not intuitive because ototoxicity symptoms don’t seem to connect directly to the cause.
Managing ototoxic chemicals in the workplace
There are several steps employers can take to minimize the risk of ototoxicity in the workplace and protect the hearing health of their employees:
1. Identify ototoxic products
The first step in managing ototoxicants in the workplace is to look for ototoxic substances in the individual chemical products being used. This is not easy, given that a typical workplace uses about 100 chemical products, each with a safety data sheet (SDS) that runs several pages long. Software can help make this process easier.
2. Determine exposure limits
Once you’ve identified that your workplace uses ototoxic products, you must research exposure limits.
3. Make chemical safety decisions
With this information in hand, you can now make decisions to:
- eliminate products where possible
- find safer substitutes, or
- implement safe handing procedures, including improving ventilation and providing proper respiratory protection or other personal protective equipment for employees who are required to handle these products for business-critical reasons.
4. Ongoing monitoring
Regular monitoring of workplace noise levels and chemical exposure is crucial. This can be done through noise measurements and air monitoring to ensure that exposure levels remain within safe limits.
5. Increase Employee Awareness
Employers should educate employees about the potential risks of ototoxicity and the importance of reporting any signs of hearing loss, tinnitus, or other ear-related problems. Explaining the requirement to use and proper wearing of personal protective equipment, where exposure cannot easily be controlled, is also beneficial.
Are you being exposed to ototoxic chemicals at work?
Ototoxicity is an emerging issue and organizations like the American Congress of Industrial Hygienists (ACGIH) are working to understand the threshold levels of exposure to these problematic chemicals. Still, there are steps that you can take to protect yourself if you’re experiencing symptoms of ototoxity.
- It’s important to speak up about it. Others may also be experiencing symptoms and the steps above can help employers improve workplace health for everyone.
- Seek external advice about your symptoms. Clinics like the Occupational Health Clinics for Ontario Workers (OHCOW) may have better understanding about ototoxicity than typical family doctors.
- If you are continuing to work and the problematic chemical is operation-critical, discuss and select a properly fitting respirator and protective clothing to prevent inhalation and/or skin absorption of the chemical until longer-term solutions can be implemented.
- If your symptoms mean that you are unable to work, the Workplace Safety and Insurance Board (WSIB) of Ontario does recognize nervous system disorder claims associated with solvent-induced neurotoxity. This avenue for support may be worth exploring.
I can tell you from experience that when you’re having dizzy spells at work, it’s hard to be productive and employees often don't want to talk about these symptoms with their employer. But for emerging health issues like ototoxicity, the key to prevention is rapid learning and sharing of knowledge and this happens faster when employees and employers work together.
Ototoxicity is a complex, debilitating condition that can be difficult to identify and address. Awareness is the first step, to be followed by a proactive approach to chemical safety that protects employees and ensures compliance with all WHMIS regulations.





