How can employers address opioid epidemic?

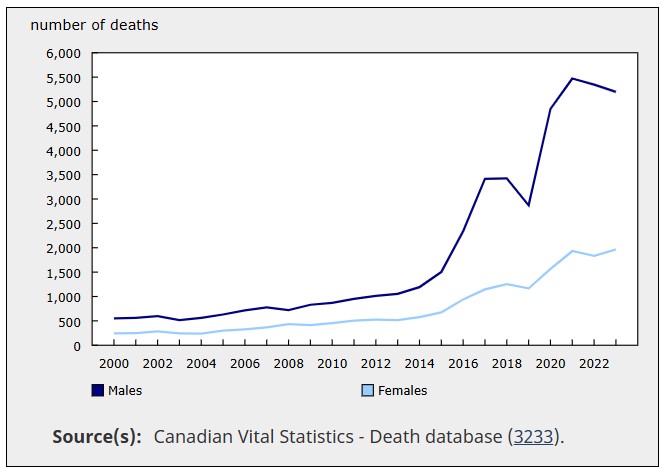
As Canada continues to deal with the opioid epidemic, the number of Canadians who have died due to accidental drug poisoning has soared over the past two decades, according to a report from Statistics Canada (StatCan).
This is true for both male and female Canadians, but the difference in the number of drug-related deaths among the sexes is enormous.
Specifically, Canada reported 549 male deaths and 246 female deaths related to accidental drug poisoning in the year 2000. By 2023, the number of deaths among males stood at 5,198. Among females, the number was 1,964.
“There has been a steady rise in the number of accidental drug poisoning deaths since 2000, with some exceptions (2003 and 2019),” said StatCan in its report. “A notable 59 per cent increase in these deaths was seen in the first year of the COVID-19 pandemic (from 4,039 deaths in 2019 to 6,412 deaths in 2020). Accidental drug poisoning deaths peaked in 2021 (7,405 deaths), before falling slightly in 2022 (7,179 deaths) and 2023 (7,162 deaths).”
 Source: Statistics Canada (StatCan)
Source: Statistics Canada (StatCan)
The opioid epidemic
“Prior to the rise observed in 2020, the largest increase in accidental drug poisoning deaths (+51 per cent) occurred during the early years of the opioid crisis, rising from 2,176 deaths in 2015 to 3,286 in 2016. The number of deaths remained high in 2017 (4,558) and 2018 (4,673), followed by a slight decrease in 2019 (4,039 deaths),” continued StatCan.
In a previous report posted in BMJ Journals, researchers found 13,702 opioid-related poisoning incidents among workers in Ontario, looking at workers identified in the Occupational Disease Surveillance System – a system linking workers’ compensation data (1983–2019) to emergency department and hospitalisation records (2006–2020) in Ontario.
And from 2016 to 2022, the rate of opioid-related deaths increased from 7.8 to 19.4 per 100,000 in Canada, resulting in almost 37,000 deaths.
“From 1 January 2006 to 31 December 2020, a total of 13,702 opioid-related poisoning events were observed among 10,064 workers (18,738,876.4 person-years), 72.1 per cent of which were male,” said the researchers from the Institute for Work & Health, Dalla Lana School of Public Health at the University of Toronto and the Occupational Cancer Research Centre.
“Just over half (53.8 per cent) of the poisoning events were accidental, 25.1 per cent were intentional and 21.1 per cent were either coded as being of unknown intent or were missing information on intent.”
In 2023, the National Safety Council noted that the opioid crisis is the fastest-growing threat to workplace safety.
In December 2024, the Supreme Court of Canada ruled that the British Columbia legislation that permits the province to bring a class action on behalf of other provincial governments and the federal government for the recovery of health care costs arising from the opioid epidemic is constitutional. In 2018 B.C. brought a claim against 49 manufacturers, marketers, and distributors of opioid products, which it alleged had contributed to the opioid epidemic by falsely marketing their products as being less addictive and less prone to abuse, tolerance, and withdrawal than other pain medications.
To combat the opioid epidemic, the Ontario government, in 2023, implemented a regulation mandating at-risk employers to have naloxone kits readily available in their workplaces.
How can employers address the opioid epidemic?
Employers have a critical role in addressing the opioid epidemic, according to the Public Health at the Milken Institute.
“Employers can play a critical role in advancing whole person health by raising awareness among employees and their surrounding communities to help prevent accidental deaths from fentanyl poisoning,” the institute said via LinkedIn.
According to one expert, addiction is often misunderstood, with many people viewing it as a moral failing rather than a disease.
"Society doesn’t like to think of it as a disease. They like to think of it as a moral failing. It's a lot easier to individualize that rather than say that it's a disease. Because if it’s cancer, we’re very empathetic towards that, right? With addiction, there’s a lot of empathy lost," said Lia Forma, MSW, relapse prevention and continuing care counsellor at Newgate 180.
For employers looking to help workers through addiction treatment, it’s important to offer flexible treatment options, such as outpatient support, to accommodate individuals who cannot take extended time off work, said Forma. Employers can also provide resources, such as Employee Assistance Programs (EAPs).
"Some HR folks will have pamphlets and stuff like that in their office to give to employees to show them, like, ‘You’re not alone. Here’s something that might help you’.”
Forma also notes that employers can follow a guide released by the Canadian Human Rights Commission (CHRC) on supporting employees with addictions.
The guide aims to “help federally regulated employers address substance dependence in the workplace in a way that is in harmony with human rights legislation,” says the CHRC.
It details the five steps employers should take in accommodating substance dependence among workers:
- Recognize the signs.
- Talk about it.
- Gather and consider the relevant medical information.
- Accommodate.
- Follow-up and adjust.
Here are the exact numbers of accidental drug poisoning in Canada per year, according to StatCan.
|
Accidental drug poisoning deaths, by sex |
||
|---|---|---|
|
Year |
Males |
Female |
|
2000 |
549 |
246 |
|
2001 |
563 |
248 |
|
2002 |
597 |
284 |
|
2003 |
514 |
244 |
|
2004 |
561 |
241 |
|
2005 |
631 |
299 |
|
2006 |
715 |
327 |
|
2007 |
777 |
369 |
|
2008 |
719 |
435 |
|
2009 |
831 |
413 |
|
2010 |
868 |
456 |
|
2011 |
950 |
503 |
|
2012 |
1,011 |
527 |
|
2013 |
1,053 |
515 |
|
2014 |
1,191 |
578 |
|
2015 |
1,503 |
673 |
|
2016 |
2,345 |
941 |
|
2017 |
3,412 |
1,146 |
|
2018 |
3,421 |
1,252 |
|
2019 |
2,870 |
1,169 |
|
2020 |
4,847 |
1,565 |
|
2021 |
5,472 |
1,933 |
|
2022 |
5,347 |
1,832 |




